Senior Dog Appetite Help
Worried because your senior dog won’t eat? This guide explains why senior dogs lose their appetite, how to safely handle prescription diets, and gentle, vet-informed steps to help your dog eat again with confidence.


Why Senior Dogs Stop Eating Prescription Diets — And How to Fix It Safely
A gentle, vet-backed guide for worried pet parents
If your senior dog won’t eat their prescription food… you’re not alone (and you’re not failing).
There’s a certain kind of panic that hits when a senior dog turns their head away from the bowl. You put the food down. They sniff. They walk away. And your heart sinks. Are they sick? Are they getting worse? Or are you accidentally “starving” them by sticking to the prescription diet?
This guide is here to take that fear off your shoulders. Using veterinarian-backed research and expert nutrition insights, this article explains:
The "Safety First" Check (When to call the vet immediately)
Why senior dogs lose their appetite (Medical vs. Behavioral)
The exact timeline of normal vs. concerning diet refusal
The five feeding mistakes that make things worse
The Three-Bucket Method for figuring out what to do next
The Topper Compatibility Matrix (what you can safely add)
The "Safety First" Check (Read This First)
Before we talk about picky eating, we need to rule out medical emergencies. Senior dogs have lower reserves than puppies, meaning they can decline rapidly if they stop eating.
If you see any of these "Red Flags," do not wait to try new food tricks. Call your veterinarian immediately.
The 24-Hour Rule: Your dog has refused to eat anything for 24 hours or more.
Nausea Signs: Lip-licking, excessive drooling, or "hard swallowing" suggesting they want to eat but feel too sick.
Sudden Rejection: Your dog ate the prescription diet happily for weeks/months and suddenly stops; this is a medical red flag, not pickiness.
Systemic Symptoms: Refusal accompanied by vomiting, lethargy, or pale gums.
The Dehydration Spiral: If your dog isn’t eating, they likely aren’t getting enough moisture. Check their gums—if they are dry or "tacky" instead of slippery, they may be dehydrated, which causes more nausea, creating a dangerous cycle.
Why Senior Dogs Lose Their Appetite
(Understanding the “why” makes everything less scary.)
A dog refusing food is never random. There are two big categories of appetite loss:
1. Behavioral or Environmental Refusal
This is common when starting a new food. It happens when the food tastes unfamiliar, the texture is weird, or the eating environment is uncomfortable.
The Aroma Factor: Senior dogs often have a weaker sense of smell. Cold food has almost no scent, which kills their appetite.
Physical Instability: Seniors with arthritis may slip on tile floors while eating. If they associate the bowl with hip pain or sliding, they will avoid it.
Pro Tip: Place a yoga mat under their bowl for traction and raise the bowl (elevated feeder) to reduce neck strain.
Whisker Fatigue: Some seniors become sensitive to tactile stimulation. Deep bowls can cause stress on their whiskers. Try a flat plate or a wide, shallow bowl.
2. Medical Refusal (Anorexia/Hyporexia)
This happens when the dog wants to eat but feels unwell. Causes include kidney disease progression, dental pain, or medication side effects.
The Difference: Behavioral refusal usually happens immediately during a diet switch. Medical refusal often happens suddenly after a period of eating well.
The Prescription Diet Rejection Timeline
(This timeline helps you distinguish between "adjustment" and "problem.")
WEEK 0–1: The Adjustment Phase (Normal Pickiness)
Most veterinary organizations recommend a slow transition over 7–10 days. In this first week, hesitation, sniffing and walking away, or spitting food out is normal.
What’s happening: The digestive system is adapting, and the brain is assessing if this new flavor is "safe."
Action: Be patient. Do not switch back to the old food immediately, as this teaches them that refusal equals "better food."
WEEK 1–2: Gentle Enhancements
If hesitation continues, this is where supportive strategies shine.
The "Sponge" Technique: For dogs with dental pain who must eat kibble, add warm water and let it sit for 20 minutes until the kibble is soft and spongy all the way through (not just wet on the outside).
Warming: Warm the food to body temperature (approx. 100°F) to unlock the aroma.
WEEK 3: The Pattern Stage (Flavor Fatigue)
If your dog eats some days but not others, or seems "bored," they may have flavor fatigue. This is common in long-term therapeutic diets.
Action: Ask your vet about switching to a different brand (e.g., Hill's to Royal Canin) within the same therapeutic class.
WEEK 4+: The “Yellow Flag Zone”
If your dog accepted the diet for weeks and then suddenly refuses it, this is not normal pickiness. This is a sign of nausea, pain, or disease progression. Call your vet.
The 5 Feeding Mistakes That Make Appetite Loss Worse
Mistake #1: Storing kibble incorrectly
Air exposure oxidizes the fats in kibble, making it go stale and lose its aroma.
Fix: Keep kibble inside its original bag, roll the top down tightly, and place the entire bag inside an airtight container.
Mistake #2: Serving food "Cold" or "Too Hot"
Cold food suppresses aroma. However, microwaving kibble can create "hot spots" that burn the mouth, creating a fear of food.
Fix: Add warm water (tested on your wrist like a baby bottle) to the food. Do not microwave the kibble directly if possible.
Mistake #3: Breaking the "Hydrolyzed" Seal
Owners often think, "Just one piece of chicken won't hurt."
The Science: Hydrolyzed diets act as a disguise—the protein is broken down so small the immune system doesn't recognize it. Adding a "whole" protein (chicken, cheese) acts like a flare gun, alerting the immune system and ruining the entire diet trial.
Fix: Nothing but the prescribed diet (and its canned version) for hydrolyzed patients.
Mistake #4: Feeding right after medication
If you pill your dog and then feed them, and the pill makes them nauseous, they will link the food to the nausea (food aversion).
Fix: Create a buffer time or ask your vet about giving meds during the meal if safe.
Mistake #5: Offering too many alternatives
If you offer three different foods in 10 minutes, you are training your dog to wait for the "jackpot."
Fix: Offer the food for 15-20 minutes. If refused, pick it up and try again at the next scheduled meal (unless they are diabetic or a very small breed—consult your vet).
The Three-Bucket Method
(A clear decision tree for what to do next)
1. The "Normal Adjustment" Bucket
Context: Week 1 of a new food. Dog acts normal but hesitant.
Action: Use "Bucket 1 Tools": Warming, hand-feeding, sponge technique, positive encouragement.
2. The "Palatability/Fatigue" Bucket
Context: Dog has been on diet for a while, eats inconsistently, or seems bored.
Action: Use "Bucket 2 Tools": Rotate to a different brand in the same therapeutic class , try canned vs. dry, or ask your vet about appetite stimulants.
3. The "Medical Urgency" Bucket
Context: Refusal >24 hours , signs of nausea , or sudden refusal after long-term acceptance.
Action: Do not force feed. Call the vet immediately for anti-nausea medication or a health check.
Advanced Vet-Approved Alternatives
If the commercial kibble simply isn't working, you still have options.
Veterinary Nutritionists: A Board-Certified Veterinary Nutritionist (DACVN) can formulate a home-cooked diet that balances your dog's medical needs with ingredients they actually like.
Compounding Pharmacies: If your dog refuses the food because of medication mixed in, compounding pharmacies can turn meds into flavored liquids (e.g., chicken or marshmallow flavor) that are easier to administer separately.
Off-Label Options: In rare cases, a vet may approve a non-prescription diet if it closely matches the required nutrient profile (e.g., low phosphorus).
❤️ A Note for the Pet Owner
If you’re reading this, you are advocating for your dog. That matters. Appetite loss is scary, but by using the Safety Check, following the Timeline, and checking the Topper Matrix, you can navigate this effectively!
The content on this website is meant to educate and support dog owners and should not be considered veterinary advice. Please consult your veterinarian before making changes to your dog’s diet, supplements, or medical care.
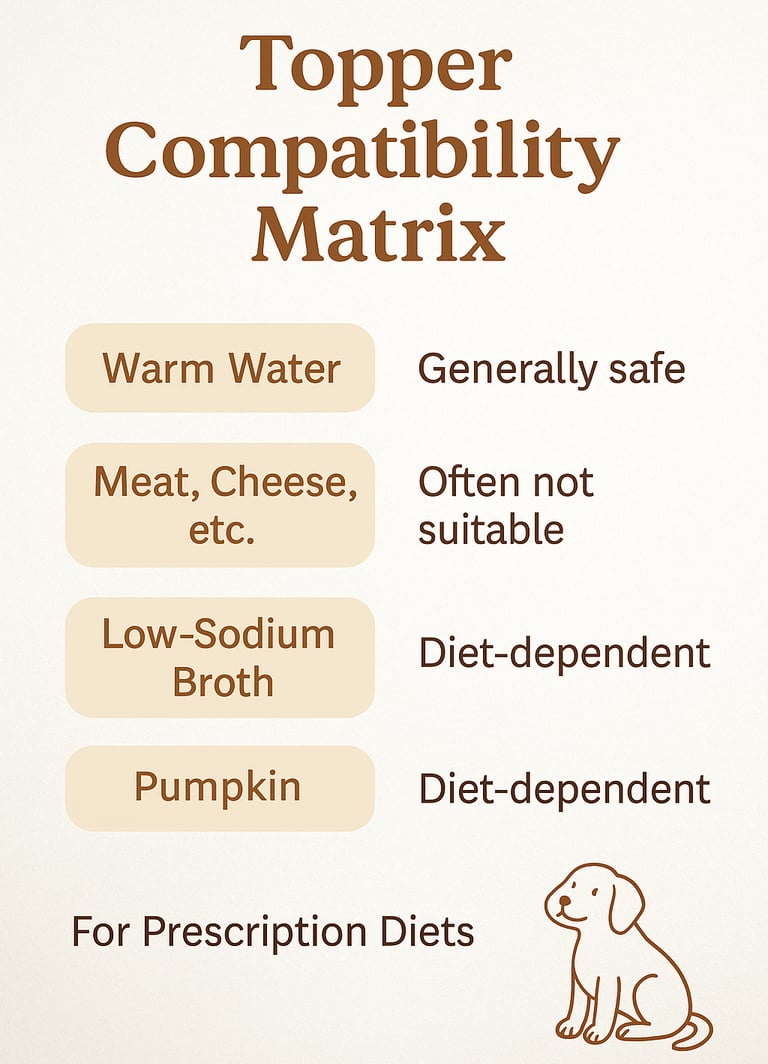

Topper Compatibility Matrix: This visual guide shows which food toppers are safe — and which should be avoided — based on your dog’s prescription diet. Use it as a quick reference to make mealtime safer and avoid accidentally interfering with your senior dog’s medical nutrition plan.
FAQs
Why do seniors lose appetite?
Senior dogs often lose their appetite due to changes in smell and taste, dental discomfort, nausea, pain, or underlying health conditions. Medications, stress, and changes in routine can also make food less appealing to older dogs.
How to handle prescription diets?
Prescription diets should be followed closely because even small changes can affect how well they work. Simple adjustments like warming the food, changing texture, or using vet-approved toppers can help improve acceptance without compromising the diet.
What gentle steps help dogs eat again?
Gentle steps include warming food to release aroma, offering a calm feeding environment, and serving smaller, more frequent meals. Patience and consistency help senior dogs feel safe and confident around food again.
When should I see a vet?
You should contact your vet if your senior dog refuses all food for 24 hours, shows vomiting, lethargy, drooling, or suddenly stops eating after previously doing well. Sudden appetite changes can signal pain, nausea, or disease progression and should be checked promptly.
Can supplements help appetite?
Some supplements may support appetite by easing nausea, improving digestion, or addressing nutrient deficiencies. Always talk to your veterinarian before adding supplements, especially if your dog is on a prescription diet or medication.
Questions?
Reach out anytime, we're here!
Join the Newsletter!
269-202-8665
© 2025. All rights reserved.